Cardiac CT provides diagnostic utility and clinical applications in cardiovascular disease
BY WAYNE M. POLLAK, MD, FACC
 |
|
 |
|
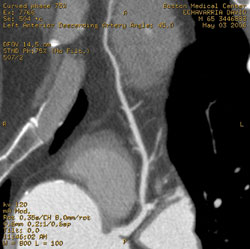
| This cardiac CT angiogram (curved multi-planar reformat) demonstrates a 20% stenosis of the left main coronary artery followed by a 40% stenosis of the ostium of the left anterior descending artery with distal luminal irregularities. |
Recent advances in imaging technologies now enable more accurate, noninvasive diagnosis of cardiovascular disease. These advances include echocardiography (newer 3-D and contrast echocardiograms), nuclear cardiac stress testing, cardiac positron emission tomography, cardiac magnetic resonance (CMR), and, recently, cardiac computed tomography (CT). Each of these imaging modalities has strengths and limitations, and each technique offers differing and complementary clinical applications.
Echocardiography is an effective imaging modality used to define cardiac function. Exercise and pharmacologic nuclear stress testing is the most widely used test for the diagnosis and risk stratification of patients with suspected or known coronary artery disease (CAD). Nonetheless, its accuracy is limited by the common presence of artifacts, resulting in a sensitivity of 88% and specificity of 74% for the detection of obstructive CAD1.
Cardiac MR is excellent for the evaluation of structural heart disease and cardiac function but is a poor study for evaluation of CAD. Cardiac CT has emerged as a robust imaging modality that provides a noninvasive evaluation of coronary arteries and cardiac function. This article reviews the diagnostic utility of cardiac CT and the means by which it is being integrated into clinical practice.
Diagnosing Coronary Artery Disease
 |
|
| This cardiac CT angiogram is a curved multiplanar reformat, demonstrating luminal irregularities (mild atherosclerosis) of the right coronary artery. |
In as much as 50% of patients, myocardial infarction or death is the initial presentation of CAD. Despite extensive research and the development of risk-prediction models, traditional risk factors often fail to predict the development of CAD or the occurrence of clinical cardiac events. An imaging modality that identifies such risk in the “vulnerable” patient has the potential to reduce the risk of CAD-related events.
Diagnostic Techniques
Coronary artery “calcium scoring,” which is performed with a noncontrast CT, is a highly sensitive technique for detecting coronary artery calcium. Calcium scoring, however, has a low specificity for detection of obstructive CAD because it does not provide an angiographic evaluation of CAD2. Although calcium scoring correlates well with overall atherosclerosis burden and CAD risk, it does not identify soft, noncalcified plaque, which may be more vulnerable to fissure or rupture and so may pose a greater risk of coronary events3.
Cardiac CT angiography, however, goes far beyond the quantification of calcified plaque burden obtained from calcium scoring. Cardiac CT, like the traditional invasive, catheter-based angiogram, uses intravenous contrast to fill the lumen of the coronary arteries. The use of multiple detectors (initially 16-slice and now 64-slice CT) and the increased rotation speed of the gantry enable imaging of the entire length of rapidly moving coronary arteries. Cardiac CT can evaluate narrowing of the arterial lumen, characterize the artery wall, and identify both calcified and non-calcified plaque.
More than 35 studies have demonstrated the high sensitivity and specificity of cardiac CT angiography for the detection of coronary stenosis. A recent study of patients with an intermediate risk of significant CAD demonstrated that cardiac CT detected noncalcified atherosclerotic disease in 30% of subjects, and in 6.2% of patients, a noncalcified plaque was the only lesion4. Mollet et al. reported the diagnostic accuracy of 64-slice CT for detecting >50% stenosis compared to the gold standard of cardiac catheterization. The sensitivity and specificity of cardiac CT were found to be 99% and 95%, respectively5. Similarly, Leschka et al. demonstrated that 64-slice CT has a sensitivity of 94%, a specificity of 97%, and a negative predictive value of 99% for classifying significant stenosis6.
Numerous studies utilizing 64-slice CT have demonstrated a consistent negative predictive value of 98% to 99% 6,7. This evidence strongly demonstrates that cardiac CT can reliably exclude the presence of significant CAD in patients with a low-to-intermediate probability of CAD. It can be used as first-line evaluation of chest pain in such patients and is particularly useful in patients who had equivocal cardiac stress testing. Thus, the high negative predictive power of CT can “rule out” obstructive CAD and help avoid the need for invasive angiography.
Additional Applications of Cardiac CT
Cardiac CT also provides accurate assessment of left ventricular function (ejection fraction, regional wall motion, and infarct identification) when compared to the gold standard, cardiac MR8, and contrast echocardiography9. Cardiac CT is helpful in the evaluation of adult patients with congenital heart disease and provides superior visualization of the anatomy of anomalous coronary arteries compared to invasive coronary angiography. In some centers, cardiac CT is used to define coronary venous anatomy accurately prior to the performance of biventricular lead placement and atrial fibrillation ablation by electrophysiologists.
Appropriate Indications for Cardiac CT
Currently accepted clinical indications are found in Table I (right) and are derived from the consensus statement written by a multidisciplinary task force of cardiology and radiology experts in cardiac CT10. The reader is referred to this article for a discussion of other clinical indications that were determined as inappropriate or uncertain indications for cardiac CT at this time. Numerous trials are currently evaluating outcome data and resource utilization in a variety of clinical presentations to clarify appropriate indications further. The use of cardiac CT in the emergency room for the evaluation of acute chest pain to exclude pulmonary embolus, aortic dissection, and obstructive CAD (coined the “triple rule-out”) is also currently under investigation. It is important to emphasize that cardiac CT as a screening test is currently not recommended because of radiation exposure and contrast administration.
Patient Selection, Limitations, and Clinical Challenges
Current limitations for the evaluation of native coronary arteries include administration of contrast and radiation exposure, the need to reduce the patient’s heart rate with beta-blockers prior to imaging, and decreased resolution in obese patients and those with significant coronary calcium. Patients with heart rates greater than 70 beats per minute have reduced sensitivity and specificity due to motion artifact. The presence of extensive amounts of calcium may reduce the ability to estimate the severity of a stenosis and thus reduce accuracy for the detection of obstructive CAD.
Coronary artery bypass grafts are imaged with excellent quality because of their larger caliber, relative lack of motion, and lack of calcification. Although current studies achieve near 100% accuracy for bypass graft evaluation, including the distal anastamosis site11, evaluation of the native coronary artery distally can prove challenging. The metal present in the struts of a stent can sometimes produce artifacts that make its evaluation by cardiac CT a clinical challenge.
Economics
Medicare recently assigned temporary current procedural terminology (CPT) codes for cardiac CT for the purpose of tracking this new technology. Local coverage determinations (LCD) for reimbursement vary widely throughout the country, and at present, reimbursement is provided in more than half of states. Currently, Florida Medicare is giving limited reimbursement under such codes and final LCD is expected to complete in 2007. The completion of clinical trials demonstrating improved patient outcomes will likely be required to gain widespread acceptance by insurance carriers.
Conclusion
Cardiac CT has a wide range of clinical applications and has demonstrated the ability to detect the presence of calcified and noncalcified plaque, as well as luminal stenosis within coronary arteries. With a consistent negative predictive power of >98%, it may become the initial test for the symptomatic, low-to-intermediate-risk patient in order to exclude obstructive CAD. Cardiac CT offers great promise in the management of coronary artery disease, but it must be used in the context of other imaging modalities and in the appropriate clinical setting.
REFERENCES
- ACC/AHA/ASNC guidelines for the clinical use of cardiac radionuclide imaging. J Am Coll Cardiol 2003;42:1318–33.
- ACC/AHA consensus document on electron-beam computed tomography for the diagnosis and prognosis of coronary artery disease. J Am Coll Cardiol 2000;36:326–40.
- Hecht HS, Budoff MJ, Berman DS, et al. Coronary artery calcium scanning: clinical paradigms for cardiac risk assessment and treatment. Am Heart J 2006;151:1139–46.
- Hausleiter J, Meyer T, Hadamitzky M, et al. Prevalence of noncalcified coronary plaques by 64-slice CT in patients with an intermediate risk for significant coronary artery disease. J Am Coll Cardiol 2006;48:312–18.
- Mollet NR, Cademartiri F, van Mieghem C, et al. High-resolution spiral CT coronary angiography in patients referred for diagnostic conventional coronary angiography. Circulation 2005;112:2318–23
- Leschka S, Alkadhi H, Plass A, et al. Accuracy of MDCT coronary angiography with 64-slice technology: first experience. Eur Heart J 2005;26:1482–87.
- Leber AW, Knez A von Ziegler F, et al. Quantification of obstructive and nonobstructive coronary lesions by 64-slice CT: A comparative study with quantitative coronary angiography and intravascular ultrasound. J Am Coll Cardiol 2005;46:147–54.
- Yamamuro M, Tadamura E, Kubo S, et al. Cardiac functional analysis with multi-detector row CT and segmental reconstruction algorithm: Comparison with echocardiography, SPECT, and MR imaging. Radiology 2005;234:381–90.
- Lessick J, Mutlak D, Rispler S, et al. Comparison of multidetector CT versus echocardiography for assessing regional left ventricular function. Am J Cardiol 2005;96:1011–15.
- ACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/SIR appropriateness criteria for cardiac CT and cardiac magnetic resonance imaging. J Am Coll Cardiol 2006;48(7). Oct. 3, 2006.
- Ropers D, Pflederer T, Rixe J, et al. Improved accuracy of noninvasive coronary angiography in patients after bypass surgery using 64-slice spiral CT. American Heart Association Scientific Sessions. Nov. 13-16, 2005 Poster 265


